The “War of the Worlds” comes home: Drug-resistant bacteria pose potential catastrophe, CDC warns
Remember The War of the Worlds movie? One of the great sci-fi flicks of the 50s. In the film, the seemingly invincible alien invaders are finally vanquished by infections from ubiquitous and innocuous (to humans) bacteria. Yesterday, the US Center for Disease Control (CDC) released a study Antibiotic Resistance Threats in the United States, 2013 that is a cautionary warning that the US and the rest of the world are engaged in a very real war of the worlds: humans vs. bacteria.
For those who are not familiar with antibiotic resistance, the World Health Organization explains antimicrobial resistance as “Antimicrobial resistance (AMR) is resistance of a microorganism to an antimicrobial medicine to which it was originally sensitive. Resistant organisms (they include bacteria, fungi, viruses and some parasites) are able to withstand attack by antimicrobial medicines, such as antibiotics, antifungals, antivirals, and antimalarials, so that standard treatments become ineffective and infections persist increasing risk of spread to others. The evolution of resistant strains is a natural phenomenon that happens when microorganisms are exposed to antimicrobial drugs, and resistant traits can be exchanged between certain types of bacteria. The misuse of antimicrobial medicines accelerates this natural phenomenon. Poor infection-control practices encourage the spread of AMR.”
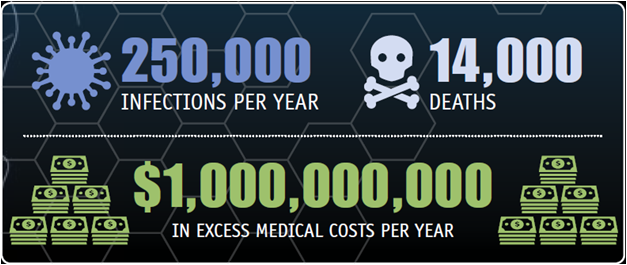
The key learning from yesterday’s CDC report: “CDC estimates that in the United States, more than two million people are sickened every year with antibiotic-resistant infections, with at least 23,000 dying as a result. The estimates are based on conservative assumptions and are likely minimum estimates.”
The report’s first section provides context and an overview of antibiotic resistance in the United States. In addition to giving a national assessment of the most dangerous antibiotic resistance threats, it summarizes what is known about the burden of illness, level of concern, and antibiotics left to defend against these infections.
The second section describes what can be done to combat this growing threat, including information on current CDC initiatives.
The third section provides summaries of each of the bacteria in this report. These summaries can aid in discussions about each bacteria, how to manage infections, and implications for public health. It also includes information about what groups such as states, communities, doctors, nurses, patients, and CDC can do to combat antibiotic resistance.
The CDC for the first time has prioritized bacteria in this report into one of three categories: urgent, serious, and concerning.
Urgent Category: Clostridium difficile: causes life-threatening diarrhea. These infections mostly occur in people who have had both recent medical care and antibiotics. Often, C. difficile infections occur in hospitalized or recently hospitalized patients.
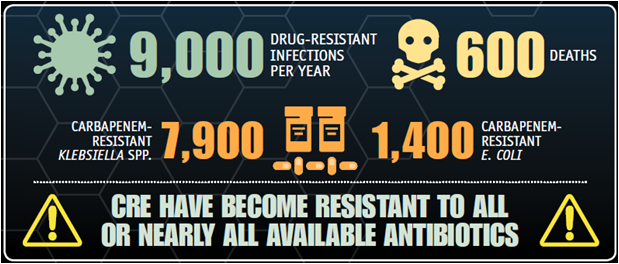
Carbapenem-resistant Enterobacteriaceae (CRE): An estimated 140,000 healthcare-associated Enterobacteriaceae infections occur in the United States each year; about 9,300 of these are caused by CRE. Up to half of all bloodstream infections caused by CRE result in death. Fortunately, bloodstream infections account for a minority of all healthcare-associated infections caused by Enterobacteriaceae. Each year, approximately 600 deaths result from infections caused by the two most common types of CRE, carbapenem-resistant Klebsiella spp. and carbapenem-resistant E. coli.
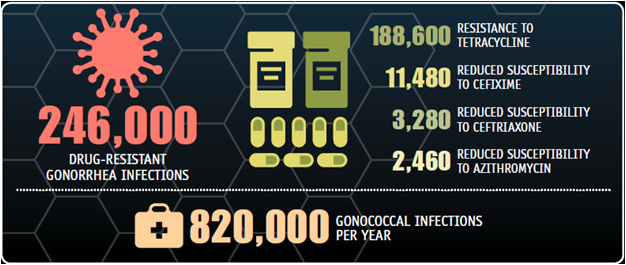
Drug-resistant Neisseria gonorrhoeae: causes gonorrhea, a sexually transmitted disease that can result in discharge and inflammation at the urethra, cervix, pharynx, or rectum. It causes severe reproductive complications.
Serious Category:
- Multidrug-resistant Acinetobacter
- Drug-resistant Campylobacter
- Fluconazole-resistant Candida (a fungus)
- Extended spectrum β-lactamase producing Enterobacteriaceae (ESBLs)
- Vancomycin-resistant Enterococcus (VRE)
- Multidrug-resistant Pseudomonas aeruginosa
- Drug-resistant non-typhoidal Salmonella
- Drug-resistant Salmonella Typhi
- Drug-resistant Shigella
- Methicillin-resistant Staphylococcus aureus (MRSA)
- Drug-resistant Streptococcus pneumoniae
- Drug-resistant tuberculosis
Concerning Category:
- Vancomycin-resistant Staphylococcus aureus (VRSA)
- Erythromycin-resistant Group A Streptococcus
- Clindamycin-resistant Group B Streptococcus
What is Being Done?
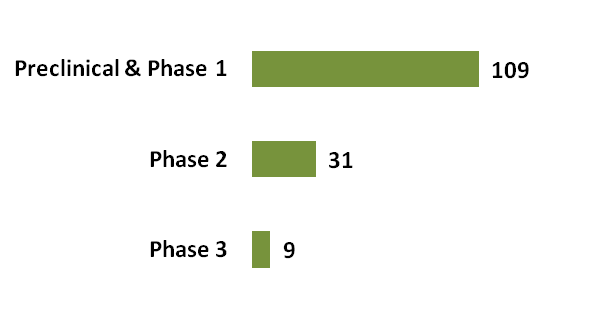
- New medicine development: according to Research and Markets 2013 industry report on antibiotics in development, there are a bit over 100 new antibiotics in the development pipeline:
- Biologists at the University of California, San Diego have developed a revolutionary new method for identifying and characterizing antibiotics, an advance that could lead to the discovery of new antibiotics to treat antibiotic resistant bacteria. The learnings from the U of C technology should help to accelerate antiinfective innovation.
- The Generating Antibiotic Incentives Now (GAIN) Act of 2011 (H.R. 2182): The GAIN Act seeks to create incentives to encourage the development of products to treat, prevent, detect and diagnose antibiotic-resistant infections. It extends the length of time an approved drug is free from competition and clarifies the regulatory pathway for new antibiotics. The key carrot in this bill is the granting of an additional five years of market protection at the end of the existing exclusivity for qualified infectious disease products. Additional benefits to the innovator are an additional six months of exclusivity to be granted for drugs for which a companion diagnostic test is cleared or approved and eligibility for Priority Review and Fast-track Approval by FDA.
- Prudent use of available antibiotics: proper use of antibiotics can help to slow the further development of new drug-resistant strains. The WHO lists the following as key in developing antimicrobial resistance:
- Lack of a comprehensive and coordinated response;
- Weak or absent antimicrobial resistance surveillance and monitoring systems;
- Inadequate systems to ensure quality and uninterrupted supply of medicines;
- Inappropriate use of antimicrobial medicines, including in animal husbandry;
- Poor infection prevention and control practices;
- Insufficient diagnostic, prevention and therapeutic tools.
Now is the time to heed the CDC’s warning and support the continued innovation in antiinfectives. The war of the worlds continues and humanity cannot afford to end up like the aliens in the film. War of the Worlds picture courtesy of Clarksville Online

[…] been killed or suppressed, usually by the use of antibiotics, causing bad bacteria, specifically Clostridium difficile, or C. […]