With all of the recent energy being spent on discussing the implementation of the health insurance portion of the Affordable Care Act (called Obamacare by some people), I wondered if there was any correlation between countries with universal health care (UHC) and those without UHC (like the United States) and how healthy the populations were in each group.
The Organisation for Economic Co-operation and Development (OECD) is composed of 34 member countries that “turn to one another to identify problems, discuss and analyze them, and promote policies to solve them”. Of these 34 countries, only five countries have less than 95% of healthcare paid by government/social health insurance: Chile (76% paid by government/social health insurance), Estonia (93%), Germany (89%), Mexico (87%), and the US (32%).
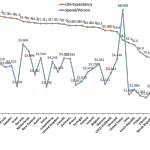
Spending versus Life Expectancy
One way to examine the effect of UHC on health is to review and compare healthcare statistics. One such obvious metric is life expectancy. The trouble with this endpoint is that there are many confounding forces on life expectancy beyond how healthcare is financed and delivered , e.g., diet, use of alcohol and/or tobacco products, level of activity, genetics, etc, but it is a place to start. Figure 1 shows the life expectancy at birth versus the percentage of gross domestic product (GDP) spent on healthcare.
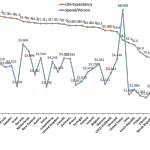
Figure 1. Life Expectancy vs. % of GDP Spent on Healthcare
As seen in the graphic, data for the OECD countries show that the life expectancy in the United States of 78.7 years is below the OECD average of 80.1. What is more remarkable is that the healthcare spend per person in the US is $8,508 versus the OECD average of $3,322. Healthcare spending per person in the US is more than 2.5 times that of the OECD average!
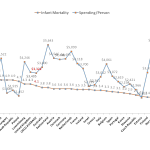
Healthcare Spending versus Infant Mortality
Perhaps there is another health measure that will provide evidence that the higher level of spending in the US system provides a superior healthcare result. Nothing could be as important to a society as the health of newborns. Looking at infant mortality statistics for the OECD reveals that the US’ higher spending has not resulted in superior infant mortality statistics as shown in Figure 2.
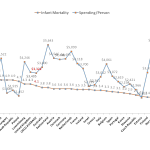
The data indicate that in spite of the highest level of spending on health, the US has the fourth highest infant mortality rates among the OECD countries; definitely not a result indicating excellence in delivering healthcare.
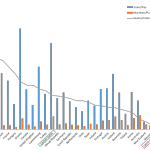
Spending and Medical Devices
How does spending on capital equipment in the US compare to the OECD countries? Looking at the number of computed tomography exams, per million population vs. total number of computed tomography scanners per million population vs. the number of exams/machine (as a rough measure of health budget efficiency, the more exams done per machine should be more fiscally efficient) shows the US about mid-pack (data were not available for all OECD countries) :
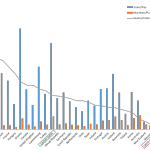
Figure 3. Relationships between CAT Scans, Machines, and Population
Stay the Course or Change?
These kinds of statistical manipulations and reviews can be performed endlessly to examine the performance of health care systems. What is clear is that the historical US health care system did not provide the best health care in the world as shown by only these few comparisons. Whether the future system in the US will perform better is certainly open to debate. I am willing to cast off the old system and embrace a system with a more universal care approach. Fingers crossed as we move forward!
Like this:
Like Loading...