It's Decision-Making, Not Geography, That Matters, September 2013
A clear, consistent, and on-going mantra in healthcare is cutting spending and improving outcomes or improving healthcare value. An historical observation has been that different areas of the United States have different healthcare spending patterns with differing health outcomes. A favorite hypothesis in improving healthcare value was to understand why these differences existed and then, on a national scale, leverage the beneficial practices that led to these differences.
"Variation in Health Care Spending: Target Decision Making, Not Geography" provides those making or selling products or services that could be paid for by Medicare or a private health insurer with reasonable and fact-based advice on developing value. This July 2013 report from The Institute of Medicine of the National Academies is likely to serve as an important information resource for future CMS and other payer strategies and actions related to the healthcare payer environment. These recommendations need to be studied and integrated into those programs that develops and provides evidence for a product's or a service's value to payers and other key stakeholders.
Significant Variation in Medicare Spending by Geography
In the report's foreword, Harvey V. Fineberg, MD, PhD, President of the Institute of Medicine (IOM) of the National Academies, stated: "Medicare's current cost trajectory is unsustainable." In order to reverse this course, periodic assessments have been made regarding Medicare spending. From past assessments of Medicare spending, it was documented that geographic variability in Medicare spending existed:
"For more than three decades, experts at the Dartmouth Institute for Health Policy and Clinical Practice have documented significant variation in Medicare spending across geographic regions apparently unrelated to health care outcomes achieved. From this seminal body of work,
an idea emerged that certain regions of the country may be uniformly more efficient than others at providing high-quality health care services. Moreover, many argue that Medicare's traditional fee-for-service reimbursement system is a major driver of both variation and waste in health care because it rewards providers based on the volume and intensity rather than the value of services delivered. Seeking strategies for reducing Medicare costs, some wonder whether cutting payment rates to high-cost areas would save money without adversely affecting health care quality for Medicare beneficiaries."
Dr. Fineberg provided two strong points on health care reform and spending:
- "...cutting expenditures through indiscriminate payment or benefit reductions would tend to shift costs to overburdened beneficiaries or diminish access to and quality of care."
- "The only sensible way to restrain costs is to enhance the value of the health care system, thus extracting more benefit from the dollars spent."
Fineberg describes the issue of geographic variability and healthcare spending:
- "The underlying premise is that certain regions of the United States spend less per Medicare beneficiary because they are more efficient providers of health care. If only researchers were able to determine what these high-value regions do that low-value ones do not, the theory goes, the core goal of the U.S. health care system (simultaneous achievement of high performance and affordability) could be achieved."
The Committee's Charge
In 2009, a group of U.S. House of Representatives members, known as the Quality Care Coalition, asked the Secretary of the U.S. Department of Health and Human Services, Kathleen Sebelius, to sponsor IOM studies focused on geographic payments under Medicare, independent of final health reform legislation, to:
- "Independently evaluate geographic variation in health care spending levels and growth among Medicare, Medicaid, privately insured, and uninsured populations in the U.S.
- Make recommendations for changes in Medicare Parts A, B, and C payments, considering findings from task (1) of the study and changes to Medicare payment systems under the ACA
- Address whether Medicare payments for physicians and hospitals should incorporate a "value index based on a composite of appropriate measures of quality and cost that would adjust provider payments on a regional or provider level basis"
The Institute of Medicine's Committee on Geographic Variation in Health Care Spending and Promotion of High-Value Care (composed of an impressive group of individuals from both public and private entities) explored a wealth of public (Medicare and Medicaid) and private (commercial insurer) data to understand better the extent and sources of geographic variation in spending and quality for Medicare and for the U.S. health care system as a whole.
Analyses of Geographic Variation
A series of analyses to quantify geographic variation in spending, utilization, and quality across various populations, payers, and geographic units; evaluate known (and measurable) factors that account for variation; and identify the types of health care services with disproportionately high rates of variation that drive total variation. Specifically, the analyses examined the roles of such factors as patient health
status and demographic characteristics, health plan, and price and market factors in accounting for geographic variation.
Their conclusions:
- "Geographic variation in spending and utilization is real, and not an artifact reflecting random noise. The committee's empirical analyses of Medicare and commercial data confirm the robust presence of variation, which persists across geographic units and health care services and over time."
What is interesting is that "areas that are high spenders in Medicare are not necessarily high spenders in the commercial market and vice versa". Further, "...spending variation in Medicare is driven by variation in utilization of post-acute services, whereas in the commercial population, price has a greater influence than utilization on overall spending variation."
- "Variation in spending in the commercial insurance market is due mainly to differences in price markups by providers rather than to the differences in the utilization of health care services."
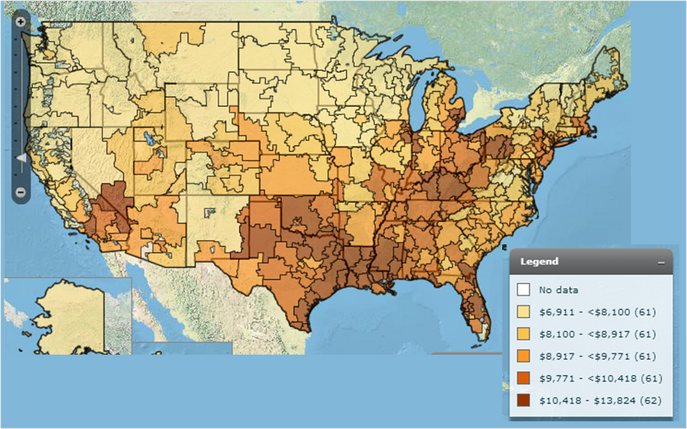
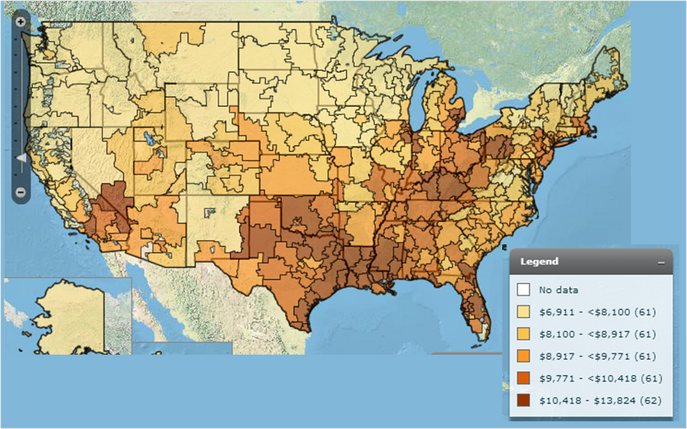
The data, illustrated in the interactive map below from the Dartmouth Atlas Project, clearly show differences in payments ($s per Medicare enrollee) by geography.
Medicare Payment Per Enrollee
For those with iPhones and other devices that cannot show the interactive map:
What is interesting is that much of the variability remains unexplained.
- "Empirical analysis revealed that after accounting for differences in age, sex, and health status, geographic variation is not further explained by other beneficiary demographic factors, insurance plan factors, or market-level characteristics. In fact, after controlling for all factors measurable within the data used for this analysis, a large amount of variation remains unexplained."
- "Variation in spending in the commercial insurance market is due mainly to differences in price markups by providers rather than to the differences in the utilization of health care services."
- "Variation in total Medicare spending across geographic areas is driven largely by variation in the utilization of post-acute care services, and to a lesser extent by variation in the utilization of acute care services."
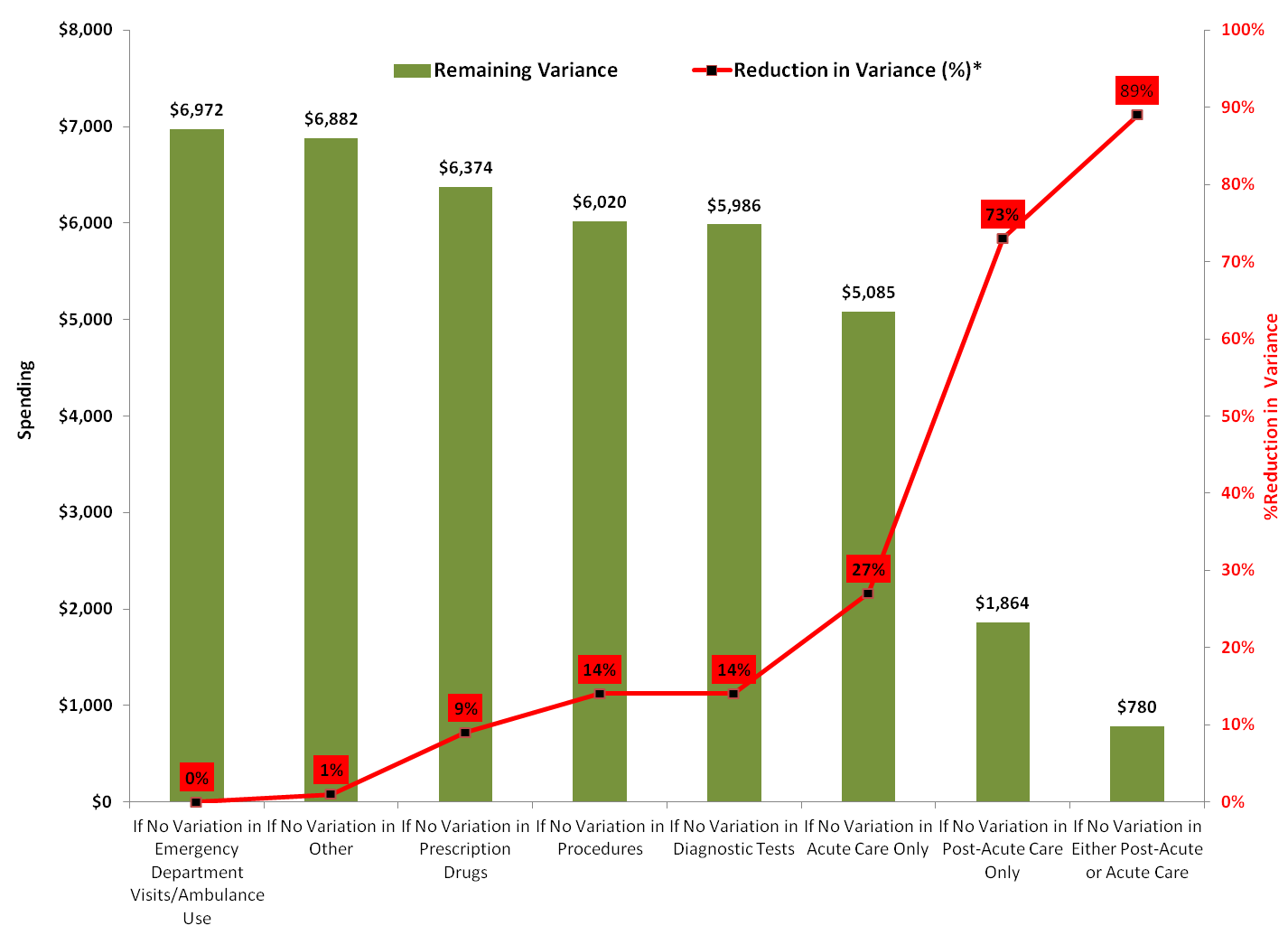
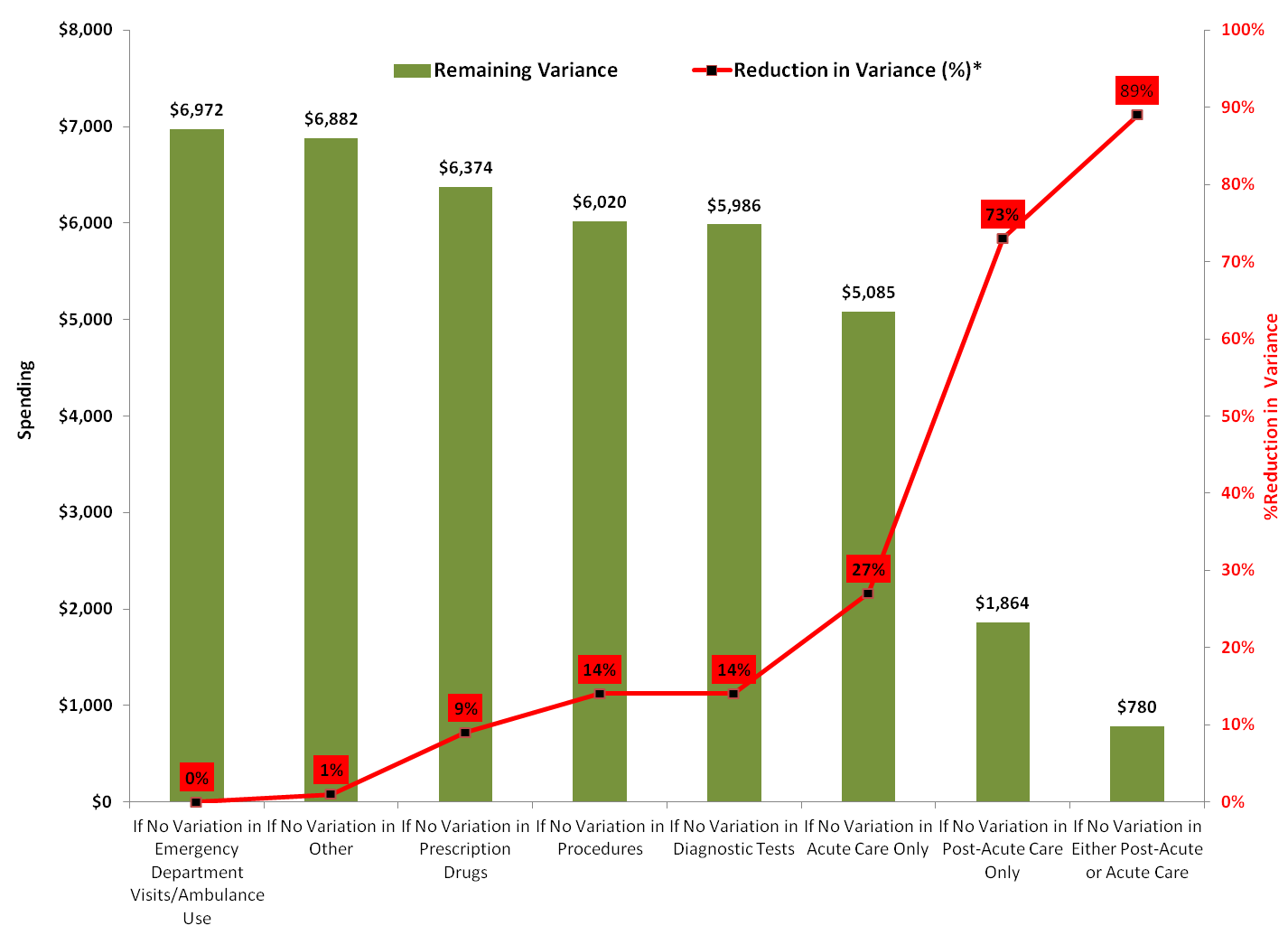
To determine the extent to which variation in particular health care services contributes to total variation in Medicare spending, the committee broke price-standardized, risk-adjusted Medicare spending into seven types of services and assessed the impact of each type of service on Medicare spending variability. The assessment revealed that only two types of spending were significant in causing variability: acute and post-acute care as shown in the figure below where their impact in reducing variability by 27% and 73%, respectively, are shown.
Proportion of Variance Attributable to Each Medicare Service Category
Key Finding: Inconsistent Relationship between Spending and Quality of Health Care
The most important finding of this research: "Correlations of spending and measures of quality for various diseases were mostly near zero, with both positive and negative signs, for both
Medicare and commercial populations." This finding indicates that (unfortunately) there exists no easily discernible pattern and/or methods of healthcare provision that will improve medical value. Instead, the variability of healthcare value is mostly derived from a complex interaction of care practices coupled with price variability.
Report Recommendations
Recommendation 1:
"Congress should encourage CMS, and provide the necessary resources, to make accessing Medicare and Medicaid data easier for research purposes. CMS should collaborate with private insurers to collect, integrate, and analyze standardized data on spending, as well as clinical and behavioral health outcomes, to enable more extensive comparisons of payments and quality and evaluation of value-based payment models across payers."
- "Variation in spending in the commercial insurance market is due mainly to differences in price markups by providers rather than to the differences in the utilization of health care services."
- "Substantial variation in spending and utilization remains as units of analysis get progressively smaller."
- "Quality across conditions and treatments varies widely within HRRs; spending and utilization across conditions are moderately correlated within HRRs."
- "HRR-level quality is not consistently related to spending or
utilization in Medicare or the commercial sector"
Recommendation 2:
Regarding geographic value: "Congress should not adopt a geographically based value index for Medicare. Because geographic units are not where most health care decisions are made, a geographic value index would be a poorly targeted mechanism for encouraging value improvement. Adjusting payments geographically, based on any aggregate or composite measure of spending or quality, would unfairly reward low-value providers in high-value regions and punish high-value providers in low-value regions."
Recommendation 3:
"To improve value, CMS should continue to test payment reforms that incentivize the clinical and financial integration of health care delivery systems and thereby encourage their:
- Coordination of care among individual providers
- Real-time sharing of data and tracking of service use and health outcomes
- Receipt and distribution of provider payments
- Assumption of some or all of the risk of managing the care continuum for their populations
Further, CMS should pilot programs that allow beneficiaries to share in the savings due to higher-value care."
Evaluating and refining the following new payment models needs to be performed:
- Value-Based Purchasing
- Patient-Centered Medical Homes
- Bundled Payment
- Accountable Care Organizations
- Multistakeholder community-based collaboratives
- Dual-Eligible Care Integration Demonstrations: The more than 9 million Americans who are eligible for both Medicare and Medicaid benefits account for a disproportionate share of Medicare expenditures: although they constitute 18% of traditional Medicare beneficiaries, they account for 31% of Medicare spending."
Recommendation 4:
"During the transition to new payment models, CMS should conduct ongoing evaluations of the impact on value of the reforms included in Recommendation 3 by measuring Medicare spending and beneficiaries' clinical health outcomes. CMS should use the results of these evaluations to iteratively improve these payment models. CMS should also monitor how these reforms impact Medicare beneficiaries' access to medical care."
Recommendation 5:
"If evaluations of specific payment reforms demonstrate increased value, Congress should give CMS the flexibility to accelerate the transition from traditional Medicare to new payment models."
Impact on BioPharma
This report reinforces how critical it is for medicine and other healthcare products and services to be able to demonstrate value. The report provides clear and reasonable guidance on how to show value to key stakeholders including payers. Now is the time for biopharma to ensure that new products and services are developed with these recommendations in mind.
How Partners in BioPharma Consulting Can Help
Contact Partners in BioPharma Consulting to see where we can assist you with crafting a development program that will deliver new products or services with demonstrable and meaningful value to key stakeholders.
Perhaps we could help you with developing a Medical Value Star for your asset and assist with forecasting and program/portfolio evaluations. We can manage a project from beginning to end, provide contracted support, or suggest talented experts from our alliance partners to help you achieve your goals. Click here for an outline of services that can be designed to meet your needs.
Links

The following links provide additional background and insights on the topics discussed in this article. I hope that you find them useful!